Benign Prostatic Hyperplasia (BPH)
World-Class Experts
We are the oldest and largest private radiology group in the Omaha/Council Bluffs area, offering patients world-class expertise in the areas of:
- Abdominal imaging
- Breast Imaging
- Musculoskeletal Imaging
- Neuroimaging
- Nuclear medicine/molecular medicine
- Pediatrics
- Trauma
- Vascular and interventional radiology
Reliable Results
The accuracy of your diagnosis largely hinges on three things:
1) the technology of your diagnostic machines,
2) the experience of the person performing your tests, and
3) the specialization and experience of the radiologist who reads your reports
We have you covered with our top-of-the line equipment and the most experienced radiology team in the area.
You're in good hands!
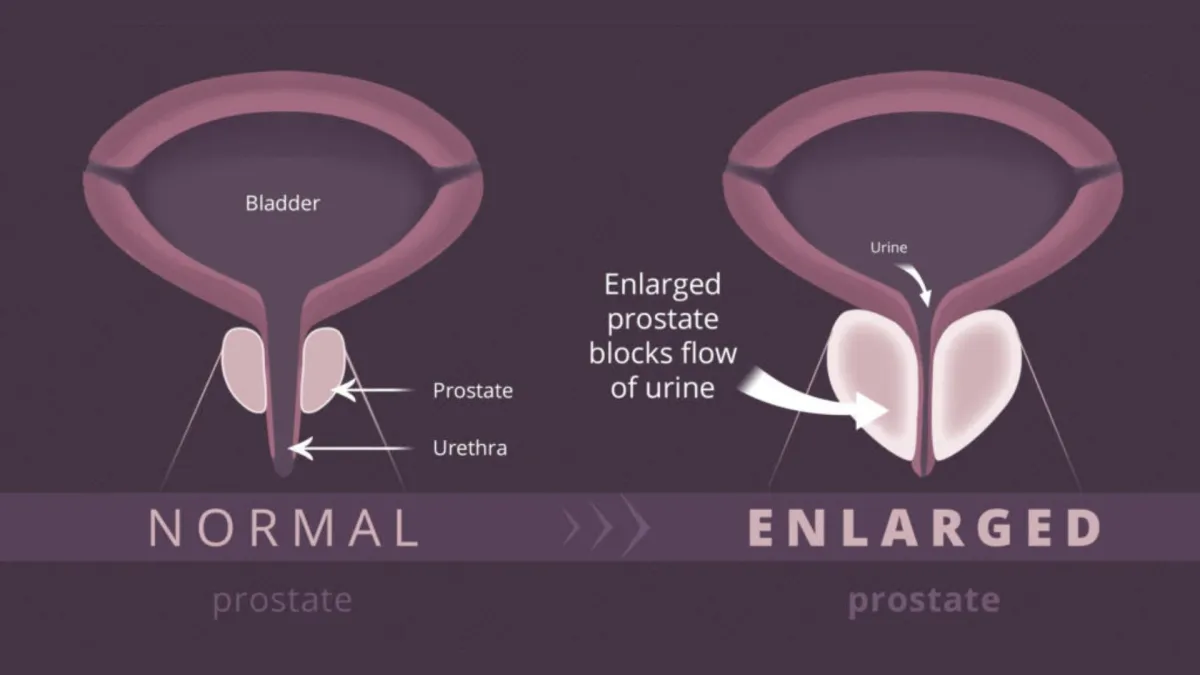
What is BPH?

Benign Prostatic Hyperplasia (BPH) is a non-cancerous enlargement of the prostate gland, which is located below the bladder and surrounds the urethra. As the prostate enlarges, it can press against the urethra and block the flow of urine, leading to symptoms such as frequent or urgent need to urinate, difficulty starting or stopping urination, weak urine flow, and incomplete bladder emptying. BPH is common in older men and can affect urinary function and quality of life.
What are symptoms of BPH?
Symptoms of Benign Prostatic Hyperplasia (BPH) include:
Frequent urination, especially at night
Sudden, strong urge to urinate
Difficulty starting urination
Weak or intermittent urine stream
Feeling like bladder isn’t completely empty after urinating
Dribbling after urination
These symptoms can impact daily life and comfort.
BPH symptoms can be divided into those caused directly by urethral obstruction and those due to secondary changes in the bladder.
Typical obstructive symptoms are:
Difficulty starting to urinate despite pushing and straining
A weak stream of urine; several interruptions in the stream
Dribbling at the end of urination
Bladder changes cause:
A sudden strong desire to urinate (urgency)
Frequent urination
The sensation that the bladder is not empty after urination is completed
Frequent awakening at night to urinate (nocturia)
As the bladder becomes more sensitive to retained urine, a man may become incontinent (unable to control the bladder, causing bed wetting at night or inability to respond quickly enough to urinary urgency).
Burning or pain during urination can occur if a bladder tumor, infection or stone is present. Blood in the urine (hematuria) may herald BPH, but most men with BPH do not have hematuria.
How is BPH diagnosed?
Summary Info
Info and more info
Info and more info
Info and more info
Info and more info
Info and more info Info and more info Info and more info Info and more info Info and more info. Info and more info Info and more info Info and more info Info and more info
The physical examination may begin with the doctor observing urination to completion to detect any urinary irregularities. The doctor will manually examine the lower abdomen to check for a mass, which may indicate an enlarged bladder due to retained urine. In addition, a digital rectal exam (DRE), which allows the physician to assess the prostate’s size, shape and consistency, is essential for proper diagnosis. During this important examination, a gloved finger is inserted into the rectum — this is only mildly uncomfortable. The detection of hard or firm areas in the prostate raises suspicion of prostate cancer. If the history suggests possible neurologic disease, the physical may include an examination for neurologic abnormalities that indicate the urinary symptoms result from a neurogenic bladder.
How does MIC treat BPH?
Other than medications and lifestyle modifications, there are a few minimally invasive procedures and surgical options to treat BPH.
Minimally Invasive Procedures
Transurethral Resection of the Prostate (TURP)
Removes part of the prostate tissue through the urethra
Laser Therapy
Uses laser energy to destroy or remove excess prostate tissue
UroLift
Implants to lift and hold the prostate tissue away from the urethra
Surgical Options
Open Prostatectomy
Surgical removal of part of the prostate through an abdominal incision, typically reserved for severe cases
Currently, the main options to address BPH are:
Watchful waiting
Medication
Surgery (prostatic urethral lift, transurethral resection of the prostate, photovaporization of the prostate, open prostatectomy)
If medications are ineffective in a man who is unable to withstand the rigors of surgery, urethral obstruction and incontinence may be managed by intermittent catheterization or an indwelling Foley catheter (which has an inflated balloon at the end to hold it in place in the bladder). The catheter can remain indefinitely (it is usually changed monthly).
About Your BPH Procedure
Minimally Invasive Procedures
Transurethral Resection of the Prostate (TURP)
This procedure involves the removal of excess prostate tissue through the urethra using a resectoscope, a specialized instrument. TURP is effective in relieving urinary obstruction and is often considered the standard surgical treatment for BPH.
Laser Therapy
Several types of laser therapies, such as Holmium Laser Enucleation of the Prostate (HoLEP) or Photoselective Vaporization of the Prostate (PVP), use targeted laser energy to vaporize or remove prostate tissue. This technique reduces bleeding and has a shorter recovery time compared to traditional surgery.
UroLift
This technique involves the insertion of small implants to lift and hold the enlarged prostate tissue away from the urethra, improving urine flow without removing tissue. It is typically performed under local anesthesia and has minimal impact on sexual function.
Surgical Options
Open Prostatectomy
Reserved for cases where other treatments are ineffective, this procedure involves making an abdominal incision to remove part of the prostate. It is generally used for significantly enlarged prostates or when other methods have failed. Although effective, it requires a longer recovery period and has a higher risk of complications compared to minimally invasive options.
Varicose
Veins
Pelvic
Pain
Non Healing Wounds
Plantar
Fasciitis
Uterine
Fibroids
Benign Prostatic Hyperplasia
Services



CT Scan
Minimally Invasive Therapies
Molecular Medicine



MRI
Ultrasound
Women's Imaging
M-F: 8:00am-5:00pm
Extended Hours Available
Upon Request